Health
Nigeria Cannot Afford 1 Doctor to 600 Patients Ratio, says FG
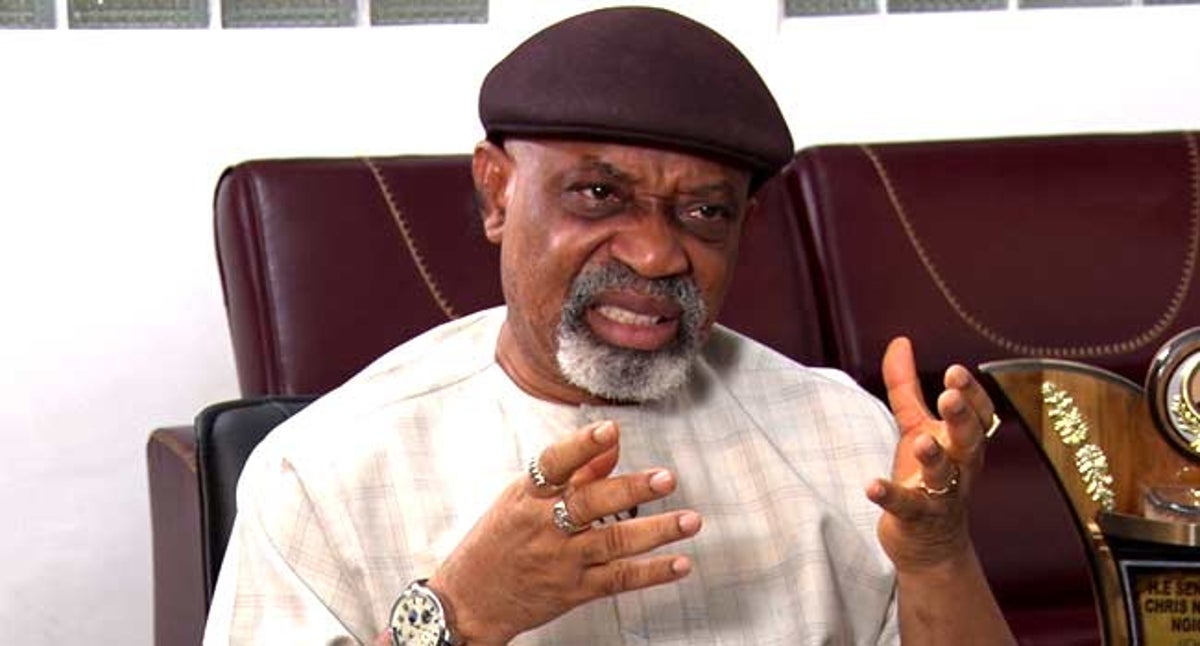
The Minister of Labour and Employment, Sen. Chris Ngige, has said that as a developing country, Nigeria was unlikely to meet the recommendation of the United Nations and the World Health Organisation’s ratio of one doctor to 600 patients.
Ngige said this at the two-day quarterly meeting of the Nigeria Health Commissioners Forum, on Friday, in Abuja.
The two-day Forum’s theme was: “Building a stronger health sector in Nigeria through collaboration and strategic partnership”.
The meeting was primarily convened to discuss how to strengthen the health system at the sub-national levels, with an overall objective of achieving Universal Health Coverage(UHC).
The Minister said: “we’re not a United Nations’ country, we are a developing country. So, when such figures are given I will tell them every rule has an exception. We are not yet there”.
“So, we shall make do with what we have. And when they’re saying he said yes. Surplus doctors. We have surpluses I keep on telling them that we have not deployed our medical manpower proportionately, and adequately as we should do”.
“How many doctors do we have in the rural areas and in the suburbs since everybody is in the townships, with a medical and dental council data showing 4,000 doctors every year. Before, it used to be 3000, before the private universities came a lot of them are not doing medicine, including Afe Babalola and others”.
“We are now in about 4000 plus, the people even trained abroad are coming back from Russia and Ukraine, and the rest of them all Medical and Dental Council of Nigeria (MDCN), is registering them”.
“So, almost everybody has come to Abuja, Lagos and Port Harcourt to stay. And we have 10,000 primary care centres that are unmanned as at the last count.”
Prof. Akin Abayomi, Lagos State Commissioner for Health, called on state’s governors to create an enabling environment for physicians in their states.
Abayomi said that there were more than 20,000 Nigerian born physicians outside the country doing extremely well.
“This is why our governors should create an enabling environment for our physicians. By now, Nigeria should not be talking about brain drain rather, it should be talking about bringing back our physicians to the country,” he stressed.
Speaking on how the state was responding to COVID-19 pandemic, he noted that Lagos state used the experience it had acquired in 2015, when it responded to the Ebola outbreak.
“This experience has helped us to effectively control the spread of the virus in the state despite, our huge population.
“We had robust data collection supporting our policy decision making. We built a system of data collection, analysis and interpretation along the lines of each pillar of the Emergency Operations Centre (EOC).
We then invested in technology to automate our data collection system through the information and implementation of the Lagos state emergency response system (LASERS), which allowed us to get data in real time for our response.
The health commissioner, however, advised that the civil service should not be used to structure or manage any-pandemic, instead, a quick policy should be developed to raise funds for effective pandemic management, otherwise, the whole system would go down.
Abayomi disclosed that Lagos was emergency ready to defeat an imminent deadlier fourth wave of the COVID-19 pandemic and future pandemics in the state, adding that the state had learnt from the first three waves.
Meanwhile, The Director-General, Nigeria Centre for Disease Control(NCDC), Dr Chikwe Ihekweazu, told the commissioners that states should play a critical role in strengthening the health security of the country.
Ihekweazu, who was represented Dr. Priscilla Ibekwe, Director, Special Duties, NCDC, added that the state had the responsibility for the health of her population, including preparedness and response to outbreaks of diseases.
“States have the resources, expertise and experience to strengthen the response to the coronavirus pandemic and other disease outbreaks in the country.
“We need stronger political commitment, leadership, and funding to fight against any outbreaks,” he added.
Dr Onoriode Ezire, Senior Health Specialist, International Finance Corporation of the World Bank Group, said that conditions for inclusion of a state in a world bank project included; “A common agreement between the Ministry of Finance and the Executive Governors on a set of transparent eligibility criteria.
“States will only be included in a project if the state’s participation would contribute to a meaningful improvement of that development indicator.
”Demonstrated commitment to reform by that state and demonstration of ongoing commitment throughout the life of a project.
“These include; meeting minimum performance criteria, adopting state legislation needed to establish an enabling environment for reform, and establishing the appropriate institutional framework to implement a reform program,” he explained.
Ezire noted that the design of multi-state operations would pay close attention to ensuring conditions for mutual accountability of both the Federal and state governments.
He commended the “Federal government for providing the enabling environment and a more level playing field for states, and states for delivering on the results to which they have committed, through their participation in the project,” he said.
In her remarks, Cross River Health Commissioner, Dr Betta Edu, who spoke on behalf of the Commissioners said that the meeting was vital to promoting experience sharing, collaboration across states, learning and fostering of sub-national development towards building a resilient health system in the country.
NAN recalls that the meeting focused on health issues such as the Basic Health Care Provision Fund; strengthening Primary Health Care; HIV/AIDS control with its multisectoral consequences; UHC, Health Insurance, as well as various high impact interventions being implemented either directly or with development partners.
The meeting also identified challenges and outlined the implementation of partnership support at the subnational level, and articulated measures to address them for adoption. (NAN)
Health
World Breastfeeding Week: UNICEF Engages Media on Field Mission

From Mike Tayese, Yenagoa
As the World mark the 2025 World Breastfeeding Week championed by World Health Organisation (WHO), United Nations Children’s Fund (UNICEF), and other partners, the Bayelsa government through the Ministry of Health last Wednesday kickoff the activities with sensitization on the importance of breastfeeding to mother and child at the Yenizue-Epie Primary Health Care Center at the heart of the state capital witnessed by who is who in the health sector, nursing mothers and expectant mothers.

During the field mission on Sunday at various churches in Yenagoa the state capital monitored by our Correspondent sponsored by UNICEF, the team visited Mount of Eternal House of Prayer Cathedral GRA Otiotio, DOC&S Church, Mount of Deliverance Okaka and CCC Palace of Mercy Arietalin Ovom in Yenagoa local government area of the state.
The team were warmly welcomed in the churches visited, addressing members of the various churches, Rose Okparan: Director Nutrition Department Primary HealthCare Board (PHCB) said World Breastfeeding Week is celebrated globally and not only in Bayelsa state every August each year.
She said breastfeeding is very important because it is the foundation of man. Breastfeeding to humans is the foundation of life. “The first breast milk that comes out when a woman delivers newly that is yellowish and creamy is very important because it contains what we called antibodies that fight against sickness and which we also called the first immunization, help the babies fight against any infection and diseases that come across the baby as it is newly born.
“The first milk also contains vitamin A to brighten the child’s eyes and it also contains protein. That yellowish one called colostrum is the richest and that is why we say don’t throw it away. It is the best and richest, it also builds child immunity, exclusive breastfeeding prevents stunted growth. Adding no water before six months is the recommended practice.
“UNICEF, WHO have carried out survey and discovered that a child breastfed for the six months exclusively are more brilliant than those that were not exclusively breastfed, it makes the brains to develop well”, she said
Grace further said, exclusive breastfeeding prevents the mother from ovarian and breast cancer, while it also helps to prevent the child from diabetes in future and several other benefits to the mothers and child.
Also speaking, the state Chairman Person of Women Wing of the Christian Association of Nigeria Bayelsa state Mrs. Grace Iyabi advised women to give their children exclusive breastfeeding for six months.
According to her, some women are afraid that their breasts will sag if they exclusively breastfed their babies, but saying whether they breastfed or not the breast will still sag because it is nature.
“It is a responsibility that God has given to everybody, it is not a choice but a priority. We have to give our children breast milk, especially exclusive breastfeeding for six months without water. Every woman is breastfed with breast milk and when you have issues of breast milk not coming contact nurses and they will tell you what to do and breastfeeding is one of the things you owe your child”.
In an interview with our Correspondent after the sensitization, Snr Apostle Michael Makpa thanked UNICEF and the Ministry of Health for the initiative about talking to churches on exclusive breastfeeding.
He said the lecture was very educational and eye opening, especially when she talked about the first milk and also how to alternate between the two breasts when breastfeeding. “It is eye opening that exclusive breastfeeding creates a lower rate of ovarian and breast cancer which most of our one younger ones should be educated about. And the belief of most of our women saying that when they breastfeed their breast will sag, she has been able to enlighten the people that either way, the breast will still sag. I think that is very very educational to us”.
Also speaking, Mother Christina Olali said, for all her children she breastfed them from zero to six months without water, only the breast milk. I even wondered that people this day within one or two months started giving their children milk instead of breastfeeding them exclusively. “Try and feed your babies with breast milk and for the lecture we heard today, I am very very happy, UNICEF and the government are trying”.
Also in the team is Gwegwe Yimuze, Head of Block DOC&S Church.
Earlier in the week, United Nations Children’s Fund (UNICEF) Field Office Enugu in collaboration with the Broadcasting Corporation of Abia held a Zoom meeting with the twelve state correspondents on Media Dialogue on Dissemination of Key Messages on the 2025 World Breastfeeding Week.
In her welcome remark, Mrs. Juliet Chiluwe, UNICEF Field Office Enugu said,2 6 out of 36 states in Nigeria have not created an enabling environment in which women can exclusively breastfeed their babies.
Saying Nigerian babies are weaned too early.
She commended 10 states which includes Lagos, Kwara, Ekiti, Oyo, Cross River, Kaduna, Niger, Ondo, Enugu, for six months’ pay maternity leave for women.
In his remark, the General Manager Broadcasting Corporation of Abia Mr. Francis Nwubani said, World Breastfeeding Week is celebrated every year in the first week of August, championed by WHO, UNICEF, Ministries of Health and civil society partners around the globe. Saying It’s a time to recognize breastfeeding as a powerful foundation for lifelong health, development, and equity.
According to him, World Breastfeeding Week shines a particular spotlight on the ongoing support women and babies need from the healthcare system through their breastfeeding journey.”This means ensuring every mother has access to the support and information she needs to breastfeed as long as she wishes to do so by investing in skilled breastfeeding counselling, enforcing the International Code of Marketing of Breast-milk Substitutes, and creating environment at home, in healthcare, and at work—that support and empower women.
“However, breastfeeding can be challenging when parents are not fully supported. Breastfeeding delivers a hopeful future not only for children, but for societies. It reduces healthcare costs, boosts cognitive development, strengthens economies, and sets children up with healthy beginnings.
“As we mark World Breastfeeding Week under the theme, “Prioritise breastfeeding: Create sustainable support systems”, WHO and UNICEF are calling on governments, health administrators, and partners to invest in high-quality breastfeeding support in so many ways especially by ensuring that all health service providers are equipped with the skills and knowledge required to support breastfeeding, including in emergency and humanitarian settings”.
Francis further said, to ensure that adequate information is passed to nursing mothers, caregivers and the general public on the numerous benefits of breastfeeding, UNICEF in collaboration with BCA Umuahia have gathered professionals from both electronic and print media for this media dialogue.
“It is indisputable that all the information about breastfeeding cannot be well disseminated without the media. You play a key role in this agenda of informing the public about breastfeeding”.
Health
UNICEF Preaches Six-month Maternity Leave Policy to Private Sector

The UNICEF Chief of Field Office in Kaduna, Dr. Gerida Birukila has appealed to the private sector to adopt a six-month maternity leave policy to support breastfeeding mothers.
Birukila made the appeal on Thursday at a “Youths Lead the Circle of Support for Breastfeeding” event, organised in Kaduna as part of the activities marking this year’s World Breastfeeding Week.
She said that working mothers face challenges in breastfeeding exclusively due to the work environment and the lack of support.
She, therefore, said a six-month maternity leave policy would enable mothers to stay at home and breastfeed their babies without interruption.
Birukila said that exclusive breastfeeding for six months can significantly reduce infant mortality rate and improve cognitive development.
“Breast milk contains all the necessary nutrients for infants, and exclusive breastfeeding can boost infants’ immune system.
“Proper nutrition is crucial for the health and development of infants.
“A well-nourished mother can provide her baby with the necessary nutrients for growth and development.
“Pregnant women should eat well, take essential supplements and micronutrients, and attend antenatal care,” she said.
Birukila emphasised the importance of exclusive breastfeeding for the first six months of a child’s life, adding that it would promote the health and wellbeing of both mothers and infants.
She said that the State Government had set an example by providing a supportive work environment for breastfeeding mothers by establishing creches in some Ministries, Departments and Agencies (MDAs).
“The state’s six-month paid maternity leave policy and crèches in MDAs are examples of best practices that can be adopted by the private sector,” she said.
The State’s Nutrition Officer, Ramatu Haruna, also highlighted the state’s support system for breastfeeding mothers.
“The state has a six-month paid maternity leave policy and crèches in MDAs, enabling working mothers to balance work and breastfeeding responsibilities,” she said.
Haruna said that the private sector could play a significant role in promoting breastfeeding.
She said that employers could provide paid maternity leave, flexible working arrangements, and other benefits that support breastfeeding mothers, helping them balance work and breastfeeding responsibilities.
She also said that the benefits of exclusive breastfeeding for six months are numerous, including reduction of infant mortality rates, improving cognitive development, and boosting the immune system.
Speaking further, Haruna said that breast milk contains all the necessary nutrients for infants, and exclusive breastfeeding can promote healthy growth and development.
She also said that employers could provide other benefits that support working mothers, including crèches or childcare services, flexible working arrangements and other benefits that support work-life balance.
“By providing these benefits, employers can help mothers balance work and family responsibilities,” she said.
Health
Nigeria’s Fight To Eliminate Hepatitis In Prisons

By Abujah Racheal
In Nigeria, estimates from the National AIDS, STIs and Hepatitis Control Programme (NASCP) show that 8.1 per cent of adults aged 15–64 live with hepatitis B, and 1.1 per cent with hepatitis C.
On a worrisome note, more than 80 per cent of those infected are unaware of their status, enabling the virus to spread silently, in homes, hospitals, and correctional facilities.
Public health experts say correctional centres are among the highest-risk environments for viral hepatitis due to overcrowding, unsafe medical practices, limited access to testing, and stigma.
According to the World Health Organisation (WHO), viral hepatitis, particularly types B and C, is a global public health threat that kills approximately 1.
3 million people each year, making it second only to tuberculosis among infectious diseases.In spite of its deadly toll, hepatitis is often overlooked, especially in low- and middle-income countries like Nigeria.
More than 91 million people in the WHO African region live with hepatitis B or C, representing 26 per cent of the global burden.
Shared razor blades, contaminated injection equipment, and poor sanitation all contribute to the spread.
When 34-year-old Malam Musa Danladi was arrested, tried and sentenced in 2022, he knew prison would be tough; but what he did not expect was that a place of punishment would become a place of diagnosis, for a disease he had never heard of.
“They called me to the clinic one morning; I was confused; the nurse said I had hepatitis B; I did not even know what that meant.”
He is one of thousands of Nigerians living with viral hepatitis, a disease that often shows no symptoms until it causes irreversible damage to the liver.
Danladi is also among the few who discovered their status within prison walls.
“We used to share everything, razors, clippers, even toothbrushes; Nobody told us we were at risk.
“Incarcerated people face a triple burden: poverty, stigma, and disease, with few resources or pathways to care,” Danladi said.
In a bid to reverse this trend, the Nigerian government, in July, unveiled Project 365, a year-long national campaign to test, treat, and vaccinate millions of Nigerians for hepatitis, including those in prison settings.
The unveiling coincided with World Hepatitis Day, with the theme: “Hepatitis Can’t Wait- Test. Treat. Eliminate.”
According to Prof. Muhammad Ali Pate, Coordinating Minister of Health and Social Welfare, Nigeria is losing between ₦10.3 trillion and ₦17.9 trillion annually to hepatitis-related productivity and healthcare costs.
“Project 365 is about saving lives and saving our economy,” he said.
Pate said that the project 365 aimed to screen every federal constituency in Nigeria, totaling 360, and to deliver curative treatment for hepatitis C as well as vaccination for hepatitis B.
He said it also sought to expand outreach to prisons, internally displaced persons (IDP) camps, rural communities, and other underserved regions.
The minister said it would ensure sustainable financing for testing and treatment, and the initiative established the Viral Elimination Fund (VEL).
Additionally, he said that the project 365 would promote local production of hepatitis diagnostics and medications, supported by tax incentives and regulatory reforms, to reduce reliance on imports.
At Kuje Medium Security Custodial Centre, a pilot hepatitis programme under the Viral Hepatitis Action in Correctional Services screened 830 inmates between December 2024 and June 2025.
Dr Ibrahim Ehizogie, a clinician with the Nigerian Correctional Services, said that many inmates were already infected with the disease while in custody.
Ehizogie said that the programme was now being scaled across Nigeria’s six geopolitical zones, with a target to reach all 300 custodial centres in the country.
However, experts warn that without continued funding, education, and policy enforcement, these gains may be short-lived.
According the 2024 INHSU Global Guideline on the Elimination of Hepatitis C in Prisons, incarcerated individuals have the same right to healthcare as the general population, and that denying hepatitis services in custody violates international human rights standards.
The guideline recommends that inmates should be tested and initiated on treatment within seven days of incarceration.
It also emphasises the integration of harm reduction services, such as safe injection practices and opioid substitution therapy, to reduce transmission.
Furthermore, the guideline advocates for peer-led education and community-based screening models to increase uptake and reduce stigma, and stress the importance of ensuring continuity of care upon release, so that individuals can maintain their treatment and health outside prison walls.
Dr Mya Ngon, WHO Team Lead for Communicable and Non-Communicable Diseases, commended Nigeria’s efforts.
Ngon said that screening must be linked to treatment, and treatment must be linked to continuity of care, even after prison.
Since his release, Daladi has become a community advocate, telling others about hepatitis, its transmission, and the importance of testing.
“I did not die in prison; so, I want to use my voice; people need to know it is not a death sentence; you can treat it; you can live; but stigma remains.
“Some people say I brought prison sickness home; some would not even shake my hand,” he said.
According to him, at present, he works in his community to support reintegration and health education, urged the government to expand outreach to ex-inmates and low-income communities.
In spite of the progress of Project 365, experts identify critical gaps in Nigeria’s hepatitis response; they say female inmates and pregnant women in custody are often excluded from routine hepatitis screening, leaving a critical gap in care.
Prof Taiwo Lateef, Professor at ABU and Africa Lead for Lifeline International, said that harm reduction services, such as access to sterile injecting equipment or safe drug treatment options, were largely absent in correctional centres.
In many cases, Lateef noted that the continuity of treatment after release remained uncertain, making long-term management of the disease difficult.
He said that youth offenders and first-time detainees typically received little to no education on hepatitis prevention, increasing their vulnerability.
Lateef said that Nigeria did not have a national hepatitis registry for prisons, making it challenging to track disease prevalence, monitor treatment coverage, or evaluate outcomes in custodial settings.
Dr Adebola Bashorun, National Coordinator for NASCP, said that without structured data and legal protections, prison health reform would remain incomplete.
Bashorun said that Nigeria’s hepatitis elimination strategy was ambitious and commendable.
He said that success would require multisectoral partnerships, political will, and a people-first approach.
According to, Dr Titilola Munkail, Technical Officer at Africa CDC, one cannot talk about ending hepatitis if one ignores people behind bars.
Munkail said that prisons were not separate from public health.
“They are central to it,” he said.
As Nigeria races toward the 2030 elimination goal, stakeholders urge the government, civil society, and citizens to act.
They say there is need for the government to institutionalise hepatitis services in all correctional facilities and primary healthcare centres (PHCs) to ensure consistent and equitable access to care. (NANFeatures)
| ReplyForwardAdd reaction |