Health
Cervical Cancer: Prevention, Causes
By Laide Akinboade, Abuja
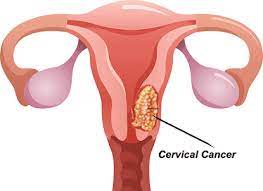
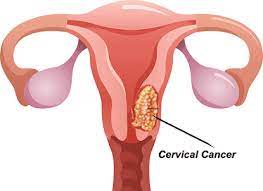
Cervical cancer is a type of cancer that occurs in the cells of the cervix, the lower part of the uterus that connects to the vagina.
Various strains of the human papillomavirus (HPV), a sexually transmitted infection, play a role in causing most cervical cancer.
When exposed to HPV, the body’s immune system typically prevents the virus from doing harm.
In a small percentage of people, however, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells.You can reduce your risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection.
Early-stage cervical cancer generally produces no signs or symptoms.
Signs and symptoms of more-advanced cervical cancer include:
Vaginal bleeding after intercourse, between periods or after menopause
Watery, bloody vaginal discharge that may be heavy and have a foul odor
Pelvic pain or pain during intercourse
Causes
Where cervical cancer begins
Cervical cancer begins when healthy cells in the cervix develop changes (mutations) in their DNA. A cell’s DNA contains the instructions that tell a cell what to do.
Healthy cells grow and multiply at a set rate, eventually dying at a set time. The mutations tell the cells to grow and multiply out of control, and they don’t die. The accumulating abnormal cells form a mass (tumor). Cancer cells invade nearby tissues and can break off from a tumor to spread (metastasize) elsewhere in the body.
It isn’t clear what causes cervical cancer, but it’s certain that HPV plays a role. HPV is very common, and most people with the virus never develop cancer. This means other factors, such as your environment or your lifestyle choices also determine whether you’ll develop cervical cancer.
Types of cervical cancer
The type of cervical cancer that you have helps determine your prognosis and treatment. The main types of cervical cancer are:
Squamous cell carcinoma. This type of cervical cancer begins in the thin, flat cells (squamous cells) lining the outer part of the cervix, which projects into the vagina. Most cervical cancers are squamous cell carcinomas.
Adenocarcinoma. This type of cervical cancer begins in the column-shaped glandular cells that line the cervical canal.
Sometimes, both types of cells are involved in cervical cancer. Very rarely, cancer occurs in other cells in the cervix.
Risk factors
Risk factors for cervical cancer include:
Many sexual partners. The greater your number of sexual partners — and the greater your partner’s number of sexual partners — the greater your chance of acquiring HPV.
Early sexual activity. Having sex at an early age increases your risk of HPV.
Other sexually transmitted infections (STIs). Having other STIs — such as chlamydia, gonorrhea, syphilis and HIV/AIDS — increases your risk of HPV.
A weakened immune system. You may be more likely to develop cervical cancer if your immune system is weakened by another health condition and you have HPV.
Smoking. Smoking is associated with squamous cell cervical cancer.
Exposure to miscarriage prevention drug. If your mother took a drug called diethylstilbestrol (DES) while pregnant in the 1950s, you may have an increased risk of a certain type of cervical cancer called clear cell adenocarcinoma.
Prevention
To reduce your risk of cervical cancer:
Ask your doctor about the HPV vaccine. Receiving a vaccination to prevent HPV infection may reduce your risk of cervical cancer and other HPV-related cancers. Ask your doctor whether an HPV vaccine is appropriate for you.
The HPV vaccine protects against the types of HPV that most often cause cervical, vaginal, and vulvar cancers.
HPV vaccination is recommended for preteens aged 11 to 12 years, but can be given starting at age 9.
HPV vaccine also is recommended for everyone through age 26 years, if they are not vaccinated already.
HPV vaccination is not recommended for everyone older than age 26 years. However, some adults age 27 through 45 years who are not already vaccinated may decide to get the HPV vaccine after speaking with their doctor about their risk for new HPV infections and the possible benefits of vaccination. HPV vaccination in this age range provides less benefit, as more people have already been exposed to HPV.
If vaccination is started before age 15, a two-dose schedule is recommended, with the doses given 6 to 12 months apart. For people who start the series after their 15th birthday, the vaccine is given in a series of three shots.
HPV vaccination prevents new HPV infections, but does not treat existing infections or diseases. This is why the HPV vaccine works best when given before any exposure to HPV. You should get screened for cervical cancer regularly, even if you received an HPV vaccine.
HPV vaccination is recommended for preteens aged 11 to 12 years, but can be given starting at age 9.
HPV vaccine also is recommended for everyone through age 26 years, if they are not vaccinated alread
HPV vaccination is not recommended for everyone older than age 26 years. However, some adults age 27 through 45 years who are not already vaccinated may decide to get the HPV vaccine after speaking with their doctor about their risk for new HPV infections and the possible benefits of vaccination. HPV vaccination in this age range provides less benefit, as more people have already been exposed to HPV.
If vaccination is started before age 15, a two-dose schedule is recommended, with the doses given 6 to 12 months apart. For people who start the series after their 15th birthday, the vaccine is given in a series of three shots.
HPV vaccination prevents new HPV infections, but does not treat existing infections or diseases. This is why the HPV vaccine works best when given before any exposure to HPV. You should get screened for cervical cancer regularly, even if you received an HPV vaccine.
Have routine Pap tests. Pap tests can detect precancerous conditions of the cervix, so they can be monitored or treated in order to prevent cervical cancer. Most medical organizations suggest beginning routine Pap tests at age 21 and repeating them every few years.
Practice safe sex. Reduce your risk of cervical cancer by taking measures to prevent sexually transmitted infections, such as using a condom every time you have sex and limiting the number of sexual partners you have.
Don’t smoke. If you don’t smoke, don’t start. If you do smoke, talk to your doctor about strategies to help you quit.
Health
Experts Seek Unified Action against Cervical Cancer
Torough David, Abuja
Stakeholders across health sectors have called for urgent, coordinated investment in prevention, equitable HPV vaccine access and harmonized health data to accelerate progress towards elimination of cervical cancer across Africa.
They made the call on Wednesday, during a panel session with the Theme ”Accelerating Cervical Cancer Elimination in Nigeria, From Policy to Practice”.
Head of Division, Maternal, Newborn, Child and Adolescent Health, Africa CDC, Dr Fidele Ngabo Gaga, highlighted its efforts to harmonise and aggregate health data across all 55 African Union (AU) Member States.
“We are developing a continent-wide data-sharing agreement and centralised repository to support data upstreaming and policy development.
“The goal is to present unified data at AU Summits, helping countries make evidence-based decisions,” Gaga said:
Prof. Imran Morhason-Bello, a leading gynaecologic oncologist from the University College Hospital, Ibadan, made a compelling financial case for prioritising prevention over treatment.
“Screening just between 2023 and 2027 will cost Nigeria N351 billion.
“But treating 10,000 women with invasive cervical cancer from 2027 to 2030 could cost us N1.4 trillion. Prevention is not only more humane, it is far more cost-effective,” he said.
Morhason-Bello also addressed innovations such as self-sampling for HPV testing, already being implemented in Nigeria through implementation science.
“Women receive a self-sampling kit, return it the same day, and positive results are treated before noon.
“It is happening in markets and schools. It is not a pilot, it is real.
“We have even developed a mobile app (available in multiple languages and offline) to guide women through the self-sampling process, increasing accessibility in low-resource settings,” he said.
External Affairs Director for MSD, Sub-Saharan Africa, Vuyo Mjekula, addressed one of the most common myths around the HPV vaccine rollout.
“Let me be clear, there is no shortage of HPV vaccines. If anyone tells you otherwise, call me directly. The real issue is equity and strategic allocation,” she said.
Mjekula recalled early proposals that included boys in HPV vaccination efforts, but warned that without careful planning, some countries would be left out entirely.
She called for one national policy that ensures equitable access to vaccines and services, especially for the most vulnerable girls.
“This is not about science alone. A dose costing N125,000 may be affordable to some, but to a woman in a rural village, it is like N10 million.
“If she must choose between survival and feeding her children, the answer is obvious,” she said.
She applauded Nigeria’s progress, noting that since the national rollout, the number of vaccinated girls across the continent has more than doubled, driven primarily by Nigeria’s leadership.
Mjekula also made an appeal for multi-sectoral collaboration, urging the involvement of private sector giants, from banks to telecoms and philanthropic foundations.
“Health is not just the government’s responsibility. We need to imagine beyond the healthcare we can afford with public funds and work toward the healthcare we want as a society,” she said.
She also called for a business case for investment in HPV prevention and cancer control, saying the task force must work hand-in-hand with all stakeholders.
“Let us go far together. If you want to go quickly, go alone. But if you want to go far, go together,” she said.
The symposium concluded with a call to integrate cancer screening into primary health care services.
It also called for the deployment of cost-effective technologies like self-sampling, addressing myths around vaccine shortages, and ensuring gender-sensitive, data-informed policies.
As Nigeria and the continent advance towards achieving the WHO 90-70-90 cervical cancer elimination targets, the message from experts was clear: “Let us do big and let us do it together”.
Health
89% of Infants Vaccinated Globally in 2024, WHO, UNICEF Warn of Risks

The United Nations agencies have reported that in 2024, approximately 89 per cent of infants worldwide, about 115 million children, received at least one dose of the diphtheria, tetanus, and pertussis (DTP) vaccine.This update comes from new national immunisation coverage data released on July 14 by the World Health Organisation (WHO) and the United Nations Children’s Fund (UNICEF).
Compared to 2023, an additional 171,000 children received at least one vaccine dose, and one million more completed the full three-dose DTP series. While these gains are modest, they reflect ongoing global efforts to protect children in spite of rising challenges.However, nearly 20 million infants still missed at least one DTP vaccine dose in 2024, including 14.3 million “zero-dose” children who never received any vaccine.This figure exceeds the 2024 target by four million, putting global immunisation goals outlined in the Immunisation Agenda 2030 at risk.WHO Director-General Dr Tedros Ghebreyesus emphasised the life-saving power of vaccines, stating, “It’s encouraging to see an increase in children vaccinated, but we still have much work to do. “Cuts in aid and vaccine misinformation threaten to reverse decades of progress.”He highlighted factors contributing to under-vaccination, including limited healthcare access, supply disruptions, conflict, and misinformation.“Data from 195 countries show 131 have consistently reached at least 90 per cent coverage with the first DTP dose since 2019. Yet, progress is stalling in 47 countries, with 22 nations seeing declines after previously meeting this target.”Tedros warned that conflict and humanitarian crises significantly undermined vaccination efforts.“A quarter of the world’s infants live in 26 fragile or conflict-affected countries, which account for half of all unvaccinated children globally.“In these areas, unvaccinated children rose from 3.6 million in 2019 to 5.4 million in 2024, highlighting an urgent need for integrated immunisation in humanitarian responses.“Immunisation coverage in 57 low-income countries supported by Gavi, the Vaccine Alliance, improved in 2024, reducing the number of under-vaccinated children by about 650,000.“Yet, some upper-middle- and high-income countries face early signs of declining coverage, which increases the risk of disease outbreaks.”UNICEF Executive Director Catherine Russell welcomed the progress but warned millions of children remained vulnerable to preventable diseases.She called for urgent action to overcome barriers such as shrinking health budgets, fragile systems, misinformation, and conflict-related access issues.Russell noted encouraging expansions in vaccines against HPV, meningitis, pneumococcal disease, polio, and rotavirus.“Global HPV vaccine coverage among eligible adolescent girls rose from 17 per cent in 2019 to 31 per cent in 2024, although it remains far below the 90 per cent target set for 2030.”Gavi CEO Dr Sania Nishtar added that while lower-income countries protected more children than ever, population growth, fragility, and conflict continued to hamper equity in vaccination efforts.She highlighted improvements in measles coverage but cautioned that it still fell short of the 95 per cent threshold required to prevent outbreaks.“Measles outbreaks nearly doubled from 33 countries in 2022 to 60 in 2024.”Nishtar stressed that funding shortfalls, instability, and rising misinformation threaten to stall or reverse progress, risking increased deaths from vaccine-preventable diseases.WHO and UNICEF called on governments and partners to close funding gaps for Gavi’s 2026–2030 strategic cycle to protect millions of children.They also urged strengthening immunisation efforts in conflict-affected and fragile settings, and prioritising locally led strategies and increased domestic investment in primary healthcare systems.Additionally, the agencies emphasised the need to counter vaccine misinformation through evidence-based campaigns.They also called for greater investment in robust data collection and disease surveillance systems to guide effective immunisation programmes. (NAN)Health
Nigeria Records 145 Lassa Fever Deaths, as Fatality Rate Increases

Nigeria has recorded 145 deaths from Lassa fever as of 2025 Epidemiological Week 25, with a case fatality rate (CFR) of 18.6 percent.
The Nigeria Centre for Disease Control and Prevention (NCDC), disclosed this in its latest report via its official website during the weekend in Abuja.
The NCDC said the week 25 figure marks an increase from 17.
6 percent reported for the same period in 2024.The report, which covered the week of June 16–22, revealed that 781 confirmed cases were reported out of 5,943 suspected cases across 20 states and 101 Local Government Areas (LGAs).
In the current reporting week, 10 new confirmed cases were reported in Ondo and Edo states with a slight increase from the eight cases recorded the previous week.
According to NCDC, 91 per cent of all confirmed cases in 2025 were reported from five states of Ondo (31%), Bauchi (24%), Edo (17%), Taraba (16%) and Ebonyi (3%).
It said that the disease continues to affect young adults predominantly, within the 21 to 30 age group most impacted. Males were slightly more affected, with a male-to-female ratio of 1:0.8.
The Nigerian public health agency, said that despite a decline in the overall number of suspected and confirmed cases compared to 2024, the rise in CFR is raising concerns among health experts.
The agency highlighted late presentation of cases, high treatment costs, and poor health-seeking behaviour as contributing factors to the increased fatality.
It said that no new infections among health workers were recorded in the reporting week, though 23 healthcare workers have been affected cumulatively this year.
The NCDC said it is currently in collaboration with partners, such as the World Health Organisation (WHO), the United States Centers for Disease Control and Prevention (US CDC), ALIMA, the Institute of Human Virology Nigeria (IHVN) and others.
The collaborations, it stated further, have intensified multi-sectoral response efforts to combat the spread of Lassa fever.
It said that, as part of these efforts, Integrate clinical trials are currently ongoing in Ondo State, with After Action Reviews (AARs) conducted in both Ondo and Ebonyi to evaluate the response to the outbreak.
The agency said that clinician sensitisation, community engagement activities and environmental response campaigns have been carried out in identified hotspot areas.
In addition, the NCDC said that it has deployed 10 national rapid response teams to various states, adopting a one health approach to disease control.
To further strengthen infection prevention and control (IPC), the agency launched an IPC e-learning platform and distributed updated Viral Hemorrhagic Fever (VHF) guidelines to health facilities across the country.
The agency said that other efforts also included active contact tracing, surveillance, media engagement and geospatial risk mapping, alongside regular webinars for clinicians and capacity-building sessions nationwide.
The NCDC identified key challenges including poor environmental sanitation and low community awareness, particularly in high-burden LGAs.
It also said that sustained efforts were needed to curb the fatality rate, ensure early detection, and improve public health outcomes.
The NCDC advised Nigerians to maintain proper hygiene, avoid contact with rodents, and seek medical help promptly when experiencing symptoms such as fever, sore throat, vomiting, or unexplained bleeding.
Lassa fever, which was first identified in 1969 in Lassa, Borno, is endemic in Nigeria, with outbreaks occurring annually.
Symptoms range from mild fever and joint pain to severe bleeding from the nose, mouth, and gastrointestinal tract.
The disease is fatal in about 20 percent of cases, particularly when treatment is delayed.
Across West Africa, hundreds of thousands are infected annually, experiencing symptoms such as fever, vomiting and, in severe cases, bleeding.
One of the most troubling complications is hearing loss, which affects about 25 percent of survivors.
The estimated fatality rate is one per cent, but during outbreaks, mortality can rise significantly, particularly among pregnant women and healthcare workers.
In spite of its significant health impact, Lassa fever remains one of the most neglected diseases, with limited resources allocated to its preventions and treatments.
Currently, no licensed vaccines exist, although around 20 candidates are in development, with the most advanced in Phase IIa clinical trials.